Process Improvement in Healthcare: Top Strategies and Skills
Polls and surveys all rank healthcare as a major public concern, whether one is looking at cost, government funding, clinical care delivery, or patient access to care.
All of these components of the healthcare “system” are susceptible to inefficiencies, waste, delays, poor results and patient (read: public) dissatisfaction when things don’t go smoothly or as desired. Continuous quality improvement is therefore an essential component of healthcare management. To accomplish this, process improvement and optimization is key.
One major area for consideration as a means of improving healthcare is optimizing clinical workflows in healthcare delivery organizations. According to the HIPAA Journal (Nov. 2021) the best possible care and improved clinical outcomes occur when clinical workflows are optimized, eliminating bottlenecks and increasing overall efficiency.
“The best possible care and improved clinical outcomes occur when clinical workflows are optimized, eliminating bottlenecks and increasing overall efficiency.”
For clinical professionals, including doctors, nurses and technical staff, every second of time is significant. Wasted time due to inefficient workflows and poor communication detracts from positive clinical outcomes. A physician might miss a specialist for a quick consult and begin the time-wasting game of phone tag. Nurses chase pages and repeat phone calls. Medical Assistants are asked to complete patient check-in questionnaires when the patient has already provided the same information in an online pre-appointment check-in. (HIPAA Journal (Nov. 2021) and recent personal experience as a patient at a major healthcare facility).
Hospital doctors reportedly waste about forty-five minutes per day due to inefficient communications
A hospital with a five hundred bed capacity loses more than $4 million annually due to communication inefficiencies (Journal of Healthcare Management)
A Joint Commission¹ study found that 60% of medical errors are due to communication failures (HIPAA Journal, Nov. 2021)
Eliminating Clinical Bottlenecks Through Process Improvement and Optimization
The patient’s journey from initial contact to admission to discharge can be slowed by inefficient communications and queues that form where processes are not staffed or handled optimally. Automation can help eliminate these bottlenecks. Adopting procedures such as check-in kiosks can help improve workflow. Avoiding duplication of tasks improves efficiency. For example, nurses in hospitals or clinics could review all prescription refill requests in one place before a physician signs off, avoiding wasted time and errors.
In order to increase ROI and make healthcare organizations truly more efficient, outdated communications systems need to be replaced. One-way channels of communication such as pagers are not the best way for physicians and staff to communicate, yet one in four hospitals in the U.S. still use pagers and fax machines. (HIPAA Journal, Nov. 2021).
“To achieve improvements, creating a culture of continuous improvement through leadership is essential. ”
To improve healthcare workflow and patient experience a modern, systems-based approach must be adopted. Multi-level strategies must be developed to address scheduling, access, diagnoses, and treatment in a systematic, automated way. Fragmented approaches must be abandoned. Disruption of old, outdated methods and analog-style technology must be allowed to occur, giving way to change and the adoption of modern, cohesive, digitized approaches to record keeping and communications. To achieve these improvements, however, creating a culture of continuous improvement through leadership is essential.
How can healthcare organizations identify workflow issues, problems and bottlenecks without also taking valuable staff time to survey and audit a myriad of functions and processes? Who is capable of coordinating overall review and summarizing the results for management in order to facilitate positive change?
HealthCatalyst suggests there are eight skills every healthcare process improvement leader must have²:
1. Communication
Communication is key. For process improvement to be effective, ideas must be clearly articulated, with concepts conveyed verbally and in writing. Listening is also critical. A leader who fails to listen is doomed to repeat old patterns and errors without finding out what the real issues are or might be. Listening and asking open-ended questions will help the leader define root causes of obstacles, errors, and issues. Listening and communicating clearly also builds trust.³
2. Trust Building
Building and sharing a vision among the process improvement leader and his or her team is critical to successful quality improvement. Staff need to know supervisors and managers have their back.
3. Coaching
Process improvement leaders also need to be good coaches. People need to understand the need for change. Otherwise change management may run into unwanted resistance to change. Staff need to be encouraged and helped to understand that they can accomplish the necessary changes in order to foster continuous quality improvement. Supporting staff is therefore essential to any successful process improvement program.
4. Understanding Process Management
The process improvement leader needs to understand the workflow, how to identify obstacles or causes of errors and waste, and how to implement the changes necessary for improvement. Having and understanding the right data is key to determining root causes of issues and finding workable solutions.
5. Understanding Care Management Personnel
To be successful, the process improvement leader has to know his people. He or she must be able to determine who does what in a process and what the necessary knowledge, expertise and skill set happen to be in a given situation. The right people need to be involved in order to resolve a specific problem.
6. Constructive Accountability and Constructive Conflict
Communication needs to be contrastive. Responding to “the way we always did it” with contrast and clarity creates an energy for change and adoption of new procedures.
7. Resilience and Persistence
Change management can be complex. Things don’t always go as planned or desired. Resistance may arise among key stakeholders or support staff, requiring patience and persistence in order to promote health change. Ask “Why will it work?” instead of “Why won’t it work?”. Getting staff buy-in is the first step. Then allowing them to proceed to the point where progress is visible will enable staff to appreciate the need for the change and to give it acceptance.
8. Seeing the Big Picture
Besides understanding the detailed, minute steps needed to create effective change, process improvement leaders need a vision of the big picture or ultimate goals. Short-term milestones or measures must be seen in the context of long-term goals and objectives. The leader must connect the dots of tasks and processes to ultimate goals.
By ensuring that a process improvement leader possesses the skills and traits discussed above, any organization seeking continuous quality improvement should see gains made in their process optimization programs. The effect can be exponential, in that leadership can then inspire others to emulate those skills and leadership traits they have seen result in positive change in their own work environment.
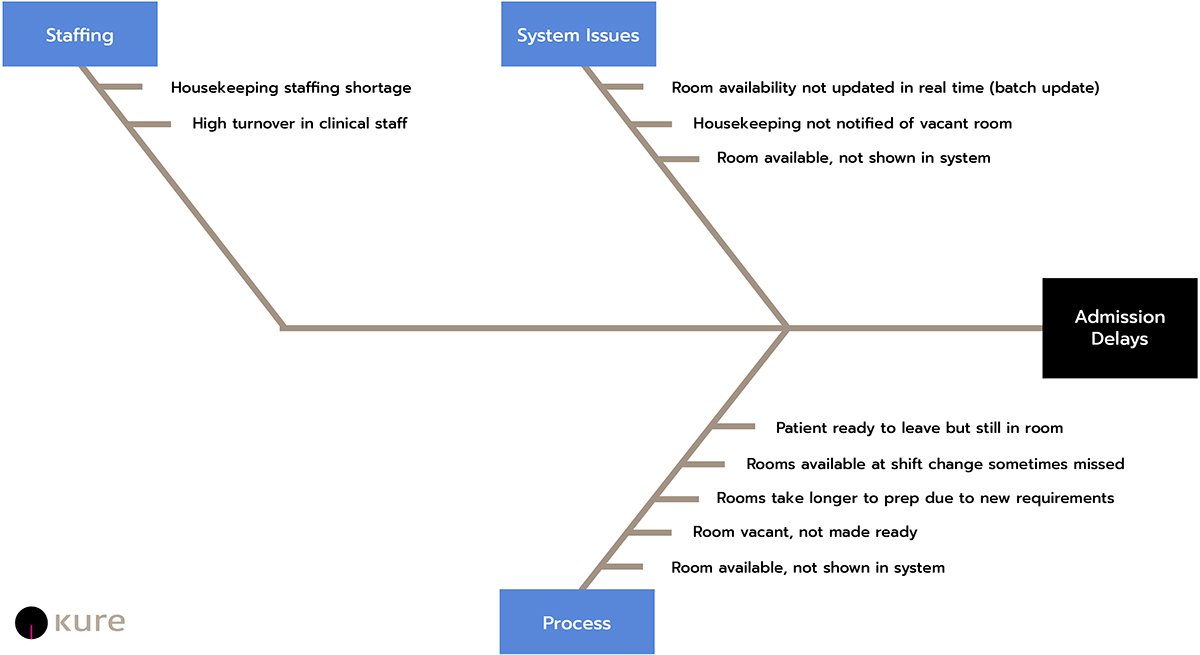
The following Fishbone Diagram shows Emergency Department issues causing patient transfer delays from the Emergency Department to the Inpatient Ward:
Process Improvement Is Not New
A number of programs and systems have been developed and used successfully to improve processes such as those affecting clinical workflow. Systems-based engineering represents one segment of this effort. The Toyota Production System was intended to improve auto manufacturing but has since spread over the years to be applied to a variety of organization processes to eliminate waste and inefficiencies. Using Value Stream Mapping, the Toyota system analyzes workflows, handoffs, and processes to create a value stream that can be modified or improved by adopting new strategies and procedures based on review of the data.
William Edwards Deming promoted other management approaches now generally known as the System of Profound Knowledge, supplemented by principles such as Deming's 14 Points for Management. (Deming is also credited with playing a key role in Japan’s industrial recovery following the Second World War, where his approach emphasized quality over production.)
“Today, everything in healthcare from delivery of care to insurance claim processing can be improved with these techniques, so long as sufficient time, staff and resources are available. The problem is the amount of time, staff, training and resources needed to create the map and determine outcomes improvement through these systems.”
The Deming Wheel or Plan-Do-Study-Act (PDSA) system is another means of optimizing organization procedures. PDSA represents a series of steps for gaining insight into the control and continuous improvement of a product or process (NCBI Resources, Nov. 2021). The key to success with this or any similar review program is integration of all the systems and subsystems involved in a particular outcome through coordinated effort among all the affected stakeholders.
The approaches promoted by Deming established a foundational base when a global network did not connect the world. The pace of operations during Deming’s tenure was sufficiently regular that organizations could be satisfied with their existing processes, could implement improvements at a modest pace, and still might not be aware of the existence of problems that were causing inefficiencies throughout their organizations. In addition, the attempt to deploy more and more software applications that purportedly ease collaboration, in many cases, simply creates an exponential growth of opportunities for failure and the introduction of new impediments.
In addition to Deming’s methods, other approaches have been developed to promote organizational optimization, such as Management by Objectives, Quality Circles, Lean and Lean Six Sigma, and Total Quality Management to name just a few. Today, everything in healthcare from delivery of care to insurance claim processing can be improved with these techniques, so long as sufficient time, staff and resources are available. The problem is the amount of time, staff, training and resources needed to create the map and determine outcomes improvement through these systems. The process can be slow and expensive.
The Kure For Improving Healthcare
Kure, with its Process Optimization Path or “POP” (™, Patent Pending) provides an efficient, easy-to-use application for individuals or teams to use to describe and map out workflow inefficiencies and communication and information bottlenecks or errors, and determine solutions for improvement. To accomplish the optimization process the Kure “stand-alone” application utilizes:
AI (Artificial Intelligence)
Algorithms
Natural language
Intelligent robotic process automation
Data mining
This cutting edge technology eliminates the need for expensive outside consultants and long-term studies in order to identify issues and root causes, and provide solutions that management can then review and adopt. A single staff person, physician, nurse or manager can use Kure to define the issues, map the flow, determine root causes, and find best solutions.
“Transparency and accountability require performance to be evaluated by reviewing data from disparate sources and cooperation by employees and senior management. ”
The single user can also involve multiple team-members by simple invitation, broadening scope and organization effectiveness exponentially. Kure helps avoid the challenge of scheduling large group meetings which often result in rescheduling and delays, therefore accelerating the improvement process. Management can then review and act on these results, optimizing processes with elegant, system-based solutions.
Transparency and accountability require performance to be evaluated by reviewing data from disparate sources and cooperation by employees and senior management.
Kure provides management with an integrated approach that produces objective results.
Monitoring post-change is essential to avoid back-sliding after new processes are adopted. This requires buy-in from all levels of staff and management, meaning education and open communication among all key players and the supporting cast.
Successful integration throughout a healthcare organization means measurable improvement in the delivery of care and the overall patient experience.
Kure invites you to become a disruptor of the status-quo in healthcare delivery. Join the Kure Digital Revolution, help optimize healthcare in your organization and establish continuous quality improvement.
Supercharge your Lean Six Sigma projects and create Ethical Efficiency™ with Kure.
¹ The Joint Commission is a private non-profit organization founded in 1951 that evaluates and accredits more than 22000 healthcare organizations and programs in the United States.
² See The Top 8 Skills Every Healthcare Process Improvement Leader Must Have, John Hansmann, MSIE, LFGIMSS, DSHS, March 30, 2018.
³ Id.