Preventing Compounded Electronic Medical Records Errors by Optimizing Processes
Instant Insight:
Digital EMRs/ EHRs enhance record transmission, storage, and patient access.
EMRs/EHRs also increase the risk of exponential errors- with potential for serious patient morbidity and mortality impact.
Physicians feel overburdened by EMR/EHR requirements that take away time for patient care, resulting in physician frustration and burn-out.
90% of physicians believe the current EMR/EHR systems are inadequate.
Optimization can improve EMR/EHR systems on a continuous basis.
“When it comes to Electronic Medical Records, 90% of doctors are dissatisfied with the way things are today.¹”
This Insight article discusses the impact of electronic medical records and electronic health records systems on patient care, hospital administration, and healthcare professionals. EMRs and EHRs have been both a boon and a bane to the healthcare industry. Digitalization can enhance efficiency, access and, at times, accuracy. However, given the nature of computer processes and the vast reach of digital technology, the same systems that create these benefits can also cause errors compounded by electronic repetition to an exponential extent. The result can be disastrous for patient morbidity and mortality and lead to physician burnout.
Physicians have been particularly impacted by the development of and new requirements for electronic medical and health records. That impact has been both positive in terms of the benefits of digital automation, but is also seen as a major contributor to physician burn-out:
“One of the key contributors to burnout involves the aforementioned EHRs. While they have the potential to make a major contribution to patient safety and enhanced coordination of care, EHRs have also radically altered and disrupted established workflows and patient interactions, become a source of interruptions and distraction and are very time intensive.²”
As we describe below, approximately 90% of physicians are dissatisfied with the status of EMR and EHR systems as they currently stand. They view the technology and record requirements as a negative in terms of excessive time spent creating potentially erroneous records and interfering with patient care.
Medicine Enters the Digital Age
Back in the ‘bad old daze’ in the mid-2000s, before digital technology swallowed medical record keeping whole, doctors kept patient care notes on 3x5 cards tucked in the front pocket of their crisp, white lab coats. At the end of the day, or perhaps every few days, the doctor would review the notes, try to decipher his or her notoriously bad handwriting, and recall patient visits in order to dictate updates to the patient’s chart. Secretaries would then laboriously transcribe the dictation into chart records for deposit in the infamous patient file room down the hall.
Today patient charts and records are referred to as either EMRs (Electronic Medical Records) or EHRs (Electronic Health Records). Digitally created, they are generally stored in the Cloud after some form of privacy encryption per HIPAA.
What is the difference between an EMR and an EHR you might ask? EMRs came first and were basically simply digital reproductions of hard-copy patient records or charts. Innovation and technological developments led to greater use and expanded detail, followed by the emergence of the Electronic Health Record, a sort of composite or amalgam of compatible records from a variety of physicians, specialists, technicians and labs. For the purposes of this article, the differences are superficial.³ We will refer to all as Electronic Medical Records.
EMRs superseded paper records on a national basis in or around 2004 when then-President George W. Bush signed an executive order intended to oversee the development of health information technology infrastructure, including both EMRs and EHRs.⁴ Ten years later the Feds began offering incentives to providers to encourage the transformation to digital records. In 2014 the incentives more or less morphed into mandates, with penalties for failing to use the technology.⁵ Many states also began implementing their own mandates for EMRs.⁶ By 2020, 89% of physicians had made the transition to an electronic system.⁷
Digital Tech: Boon or Bane?
That transition has not been entirely smooth or without glitches and costs. Most physicians report issues or problems with their EMR or EHR systems. In a survey conducted by Deloitte, only 10% of doctors were satisfied with the way things are with respect to digital records.⁸ In the same study, 35% of physicians reported a lack of user-friendliness as a major issue.⁹ Many physicians report “burnout” with the current digital systems, with time wasted or too many errors. As SelectHub has reported, “physicians hate EMRs.”¹⁰
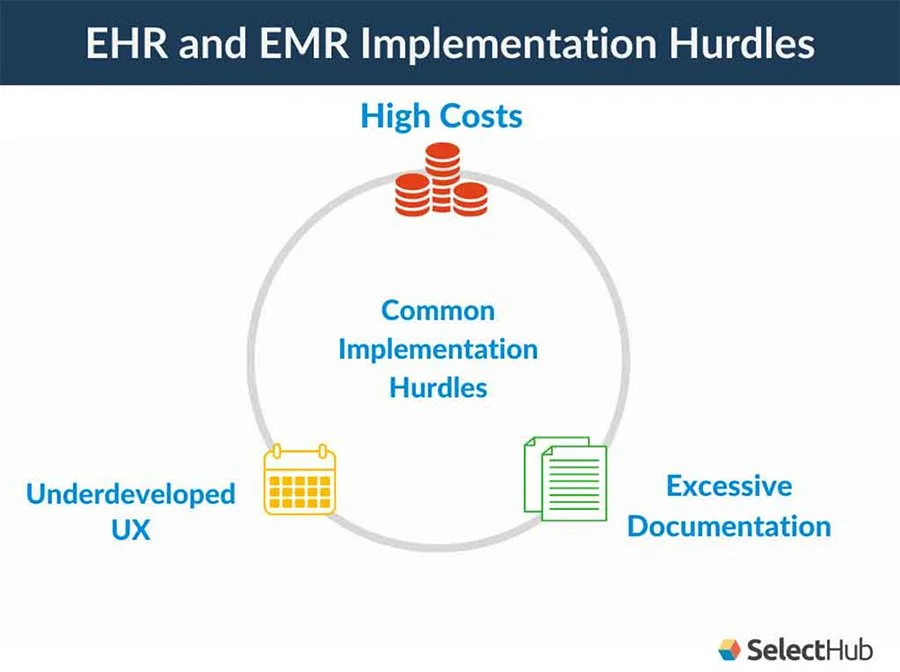
As a result of physician complaints and patient dissatisfaction, many institutions have undertaken review of their digital record systems in terms of the impact on physician time and patient care, error rates, and patient outcomes. The results have been mixed, but most would agree that the systems can and should be improved. Cost, errors, accessibility and lack of user-friendliness have all been cited as reasons for change.¹¹
Source: SelectHub
Technical problems with EMRs not only hamper care and waste time in the eyes of physician-users, but can result in significant costs as well. Kimberly Reich, Privacy and Compliance Officer for Lake County Physicians, recently stated: “Cost continues to be the most significant and major barrier that affects healthcare practitioners from adopting EMR.” This is particularly problematic for smaller clinics and practices.¹²
“The medical record has become unreliable due to inappropriate use of features like copy-paste. With many doctors, you don’t bother reading their note because you don’t know if you can trust it. This creates inefficiency because you have to go to the source to verify it. It’s a big safety and efficiency issue. This means that patient records are not always correct, reducing the value of the EMR system overall and contributing to errors in patient care. The future of health EMR needs to change, and judging by some of the issues currently facing it, it needs to change in big ways.”
Most practitioners believe EMRs and EHRs have the potential to improve with greater patient engagement, accessibility and accountability.¹³ Consumer activism and patient advocacy groups have put pressure on hospitals and clinics as well as insurers to provide greater patient access and input to their records.¹⁴ The need for user-friendly and accurate record-keeping systems has therefore never been greater.
5% of all Google searches relate to healthcare.
Most physicians believe improvement is needed in their EMR/EHR systems.
The majority of patients search the Internet for their healthcare information.
“Sadly, most EMR software is terribly inadequate. They were built on obsolete platforms with little thought dedicated to user experience.¹⁵”
Many EMR/EHR systems are “stand-alone” and do not easily integrate with other information systems. This frustrates providers as well as patients. Accessibility is essential, which means integration and interoperability, in addition to searchability and ease of use.¹⁶
The Boomerang Effect
Digitalization has improved efficiency and accuracy to some extent, but it has also resulted in magnification of errors and negative patient impacts. Computer error has created the opportunity for unintended prescribing errors leading to overdose in some instances. In one such case, a doctor at UCSF hospital prescribed a drug for a pediatric patient in a dosage in milligrams, as he normally would for an adult. He did not realize the computer needed the dose to be given in milligrams per kilogram for a child. The computer issued a warning of the excessive dose, but because the computer had previously issued many “false positives,” the doctor ignored the warning. The pharmacist did the same. A robot packaged the erroneous drugs for dispensing to the patient. The nurse who administered the dose realized it was a gross overdose, but the computer assured her that both the doctor and pharmacist had signed-off. The teenage patient experienced a massive overdose.¹⁷
The Pennsylvania Patient Safety Authority in Harrisburg found that from January 2016 to December 2017, electronic health-record systems were responsible for 775 problems during laboratory testing in the state, with human–computer interactions responsible for 54.7% of events and the remaining 45.3% caused by a computer.¹⁸
“The combination of excessive documentation expectations and poor UX results in physician burnout and overwork. Burnt out physicians, nurses and other staff often seek ways to reduce their data entry workload, resulting in mistakes or cutting corners.²⁰”
In 2017 eleven chief executives of US medical centers wrote that, although electronic health records can improve patient safety, these systems had “radically altered and disrupted established workflows and patient interactions” for physicians, and had become a main contributor to the growing problem of physician burnout.¹⁹
Science and Technology author Jeff Hecht in Nature suggests that one way to overcome the keyboard problems of physicians might be to utilize the growing number of programs that enable machines to process the spoken word. He cites Gregg Meyer, Chief Clinical Officer at Partners Healthcare, which runs several Boston-area hospitals, in support of using “natural language” to “rehumanize medicine” so that physicians can spend more time with patients (and less glued to laptops).²¹
Optimizing EMRs and EHRs would seem an obvious tool in the struggle to improve medical record systems and medical care. Today there are many organizations with consultants dedicated to reviewing these systems and suggesting improvements, all with a significant cost in terms of staff time and hard-bitten institutional resources. Is there another, more efficient way to improve this critical facet of our healthcare system?
Fortunately, there is an alternative. Kure, with its Process Optimization Path™ has developed a digital application accessible to anyone in healthcare to provide a fast and efficient means to review information processes, including EMR and EHR processes, identify obstacles, errors and waste, to develop workable, replicable solutions.
Kure utilizes an elegant combination of AI, algorithms, auto-robotics, machine learning, data mining and natural language to provide near-instantaneous responses and results for optimization projects defined and developed by the user following the Kure prompts. It eliminates the need for time-consuming and costly review with expensive outside consultants and dedication of substantial employee training time to learn the “hows” and “whys” of optimization and then implement the learning.
The Kure Solution*
Kure emphasizes process. When we find problems with EMR/EHR systems, it's all too easy to attribute it to human error. People are certainly involved or nothing would be accomplished. Often the people are simply trying to do the best they can with a process which may not only be inadequate, but may actually be working against them.
When technology is added to inadequate processes the problems are inflamed. Now, we find ourselves in the situations described earlier in this article. People are working harder and getting less accomplished due to processes and technology that are not optimized to meet the needs of the patient and enable staff to provide timely quality care. Kure’s Process Optimization Path™ provides the methods and guidance to optimize the integration of people, process, and technology.
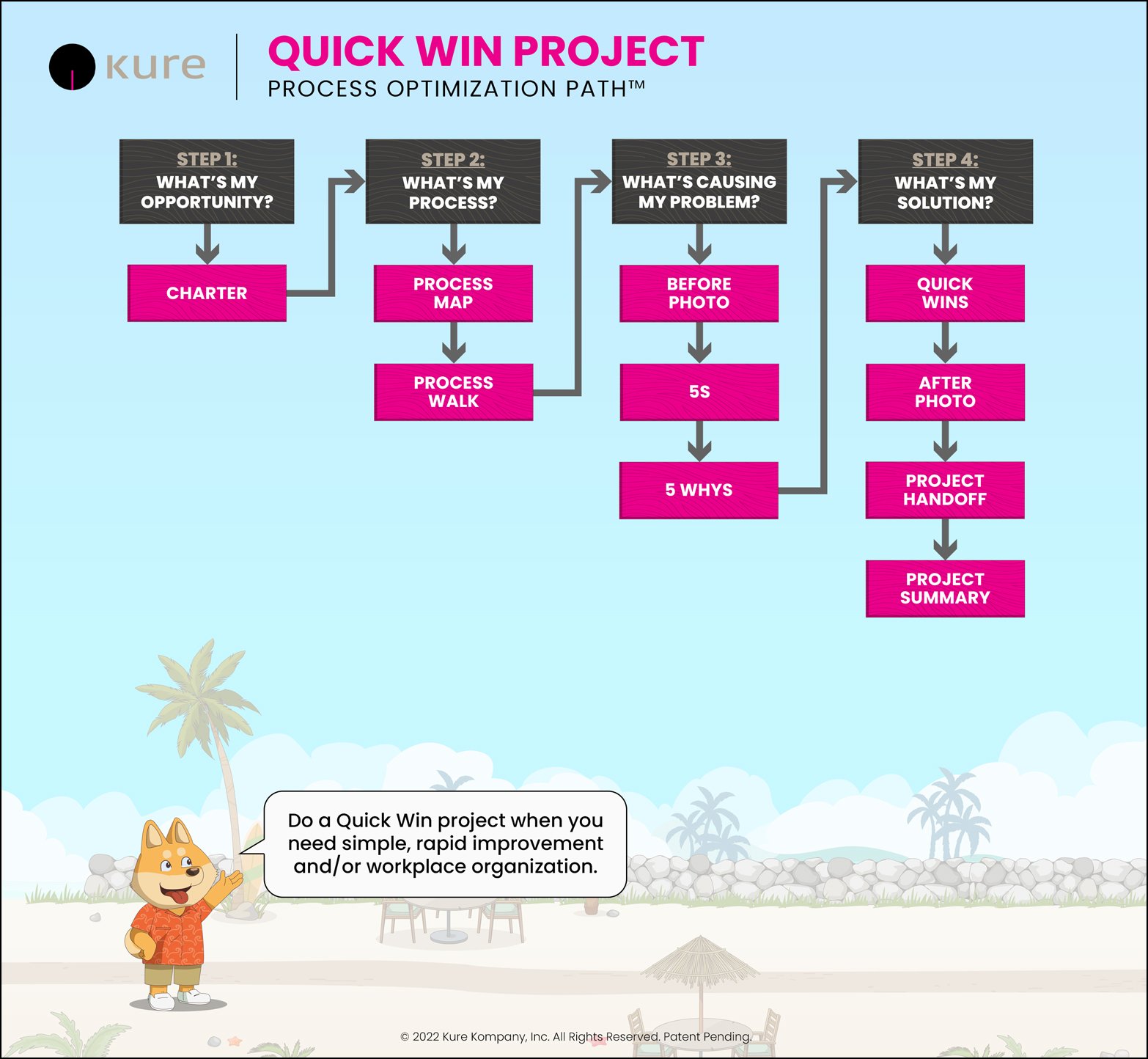
Quick Win Pathway
Kure's Quick Win pathway provides a quick and easy way to document and survey processes, looking for specific EMR/EHR problems along the way. This includes mapping the process and walking the process. Those who work in a process often think they know the process well, but they may only know their part well. When all the participants collectively map the process, a more complete understanding happens.
“During [the] Process Walk, problems can often be witnessed as they develop. When this happens the cause of the problem is usually not far away. The user is then well-positioned to find a solution.”
Once the process is mapped, Kure asks that the user walk the process to both confirm that it really operates as mapped, and to find improvement opportunities. During this Process Walk, problems can often be witnessed as they develop. When this happens the cause of the problem is usually not far away. The user is then well-positioned to find a solution.
Suspected causes are refined using the 5 Whys, which often suggests simple and easy solutions, called Quick Wins. Ideas are tested and an Implementation Plan is built.
The Quick Win pathway is a quick and easy way for rapid improvements — often in a day or two. For more complex issues, Kure’s Root Cause Exploration™ pathway provides the rigor needed for the tougher problems.
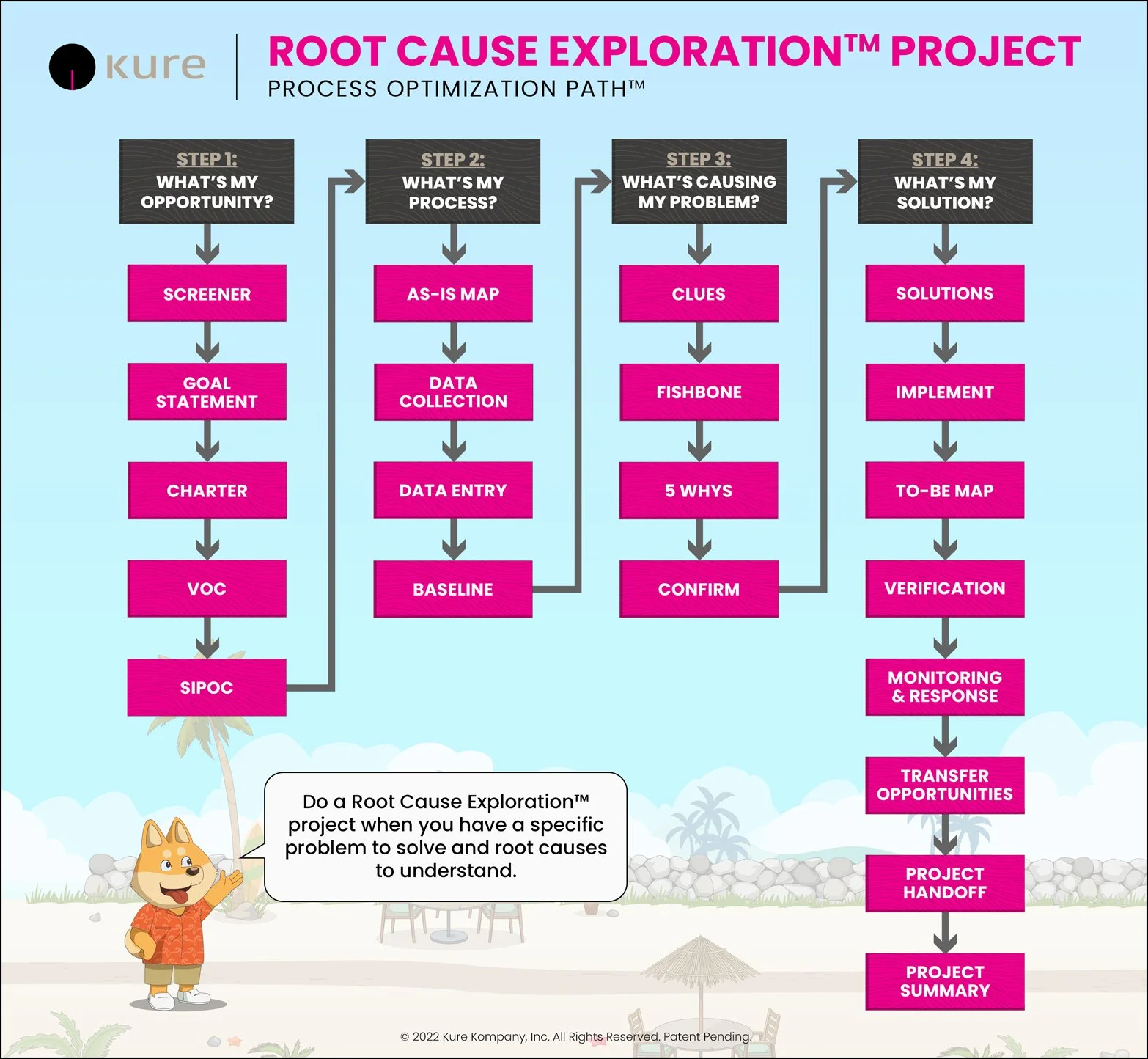
Root Cause Exploration™ Pathway
The Root Cause Exploration™ pathway addresses complex problems with numerous causes that are unknown, which is often the case in EMR/EHR processes. This pathway provides step-by-step guidance to fully analyze the problem, verify the root causes, implement targeted solutions, and sustain performance. The Root Cause Exploration™ pathway provides a flexible and robust approach to solving various problems. The better you define the problem the faster and more effective the project will be. Kure helps you create that focus and drive, speed and effectiveness.
In the case of the EMR/EHR, the two problems often encountered are the excessive time required to document and the inaccuracy of the documentation. While these issues are interrelated, selecting one as the primary focus will greatly increase the project's speed and effectiveness. It is often a difficult decision to focus on one—time versus accuracy. However, the focus on one has the added benefit of improving the other. Kure guides you to define the priority problem and set the project up for success.
For example, if your focus is to reduce the time and effort required and therefore reduce the staff frustration and burnout, then Kure will help identify where and how these problems occur in the process and technology. Many processes grow overly complex and cumbersome over time and need to be “refreshed,” tossing out elements no longer required. Adding technology to these processes before they are streamlined can be disastrous.
“The better you define the problem, the faster and more effective the project will be.”
With the tools of Baseline Analysis, Non-Random Pattern Detection, Fishbone Diagrams, and 5 Whys embedded in the Root Cause Exploration™ pathway, root causes are verified with facts and data. This is a critical step to solving complex problems and Kure will guide you to eliminate these causes and improve the flow of work, leading to reduced cycle time, increased productivity, and improved accuracy.
If the focus is on improving the accuracy of the record, then Kure guides you to identify the sources of errors. A process that produces a lot of errors often has numerous errors throughout that require “fixing” along the way. This causes internal rework to correct things already completed. This extra work, which can be tremendous, leads to staff frustration and burnout, much like the EMR/HER examples discussed earlier. This extra work, and time, is often called the hidden factory and is common in both manufacturing and service processes.
In this pathway, you’ll target your most painful sources of rework, understand the root causes, and develop targeted solutions. Again, the analysis tools embedded in the Root Cause Exploration™ pathway are critical to eliminating the most painful sources of rework. This focus provides leverage to make improvements and realize breakthrough results.
Regardless of the priority, reducing time, or increasing accuracy, Kure’s Process Optimization Path™ will guide you to optimize processes and technology to provide better patient care and empower care providers.
Supercharge your Lean Six Sigma projects and create Ethical Efficiency™ with Kure.
¹ See Future of Electronic Medical Records, Experts Predict EMR Trends in 2022. Divya Dugar, SelectHub, 2022.
² See Physician Burnout Is A Public Health Crisis: A Message To Our Fellow Health Care CEOs
³ See EHR vs EMR: Comprehensive Comparison of the Difference Between Them.Evan Heier, SelectHub, 2022.
⁴ Id.
⁵ See USFHealth, Morsani College of Medicine, Federal Mandates for Healthcare, Digital Record-Keeping Requirements for Public and private Healthcare Providers, February 16, 2017.
⁶ See State EHR Mandates, Physicians Practice, August 17, 2010.
⁷ See Future of Electronic Medical Records, Experts Predict EMR Trends in 2022. Divvya Dugar, SelectHub, 2022.
⁸ Id.
⁹ Id.
¹⁰ Id.
¹¹ Id.
¹² Id.
¹³ In 2017 California enacted the Patient Access to Health Records Act
¹⁴ Id.
¹⁵ Id.
¹⁶ See footnote 5, supra.
¹⁷ Id.
¹⁸ Id. See also Liberatore, K. Pa. Patient Saf. Advis. 15 (Suppl.), 16–24 (2018).
¹⁹ Id. See also Physician Burnout Is A Public Health Crisis: A Message To Our Fellow Healthcare CEOs
²⁰ Id.
²¹ See The Future of Electronic Health Records
* Kure provides a digital system for optimizing processes, including record-keeping, However, results may depend on individual applications and may vary according to the data provided.