Nursing Crisis: How Process Optimization Helps Hospitals Respond to COVID-19
Instant Insight:
Nursing burnout fuels exodus with retirements and resignations
Nursing shortages cause increased patient care errors and staff stress
Remedies include redirection of staff resources, and tapping non-traditional resources (moving non-clinical employees into patient care roles)
Volunteerism and recruitment/retention as critical components
“COVID-19’s latest surge exacerbates long-standing forces driving nursing shortfalls, prompting an all-hands-on-deck scramble to maintain patient care.¹”
The COVID-19 pandemic has disrupted the delivery of healthcare services in a variety of ways on a global scale. Here in the U.S., no single aspect of healthcare has been more profoundly impacted than the delivery of nursing services. The long-term ramifications for healthcare are significant, affecting patients, practitioners, hospitals, insurers and government.
First it was the COVID Delta variant surge filling Emergency Rooms and Intensive Care Units in the Summer and Fall of 2021. Then the virulent, ultracontageous Omicron variant hit the population and the medical workforce, creating shortages among critical hospital staff as mandatory quarantines resulted in reductions in available nursing personnel and related staff resources.
The increased stress of dealing with the COVID crisis on a daily basis has led to unprecedented early retirements as well as burn-out resignations among nursing and other critical care personnel.² In addition to ERs and ICUs, vacancies are causing stress in respiratory therapy, medical tech, environmental services (cleaning) and food services.³
According to Barron’s, the nursing shortage “compounded by the COVID-19 pandemic will likely persist for years, driving up wages and healthcare costs while suppressing spending on non-nursing Hospital expenses such as equipment or new medical technologies...”.⁴ Thus a COVID-induced staff shortage impacting critical care nursing has also produced a shortfall of funds available for new medical technology, services and innovation, all at a yet unknown cost to our healthcare system and patient care.
Patient Safety at Risk
Low nurse-to-patient ratios can lead to medication errors and higher morbidity and mortality rates. The patient risk of infection can increase by up to 15% when a unit is understaffed. Readmissions also climb in the pediatric population when there is a shortage of nursing staff.⁵
Confronted with the global pandemic, nurse burnout and patient dissatisfaction, many hospitals are struggling. In addition, studies have shown that nurses are experiencing increased workplace violence and abuse, leading to further burnout, resignations and retirements. Heavy workloads and the stress of caring for dying patients increase the intensity of the crisis. One estimate from 2018 found that nurse turnover cost the institution(s) $44,000 per nurse.⁶
Regional differences can also exacerbate the impact of the nursing shortage. Rural areas are more likely to face severe shortages than urban and suburban communities.⁷ In one survey, nearly 99 percent of rural hospitals reporting experienced staffing shortages, with 96% saying filling nursing positions was the most difficult.⁸ Patients in rural areas may have to travel for hours in order to find needed care.⁹ Vox reports that one in four hospitals said a lack of nurses forced them to suspend critical services, including newborn delivery, chemotherapy and colonoscopies.
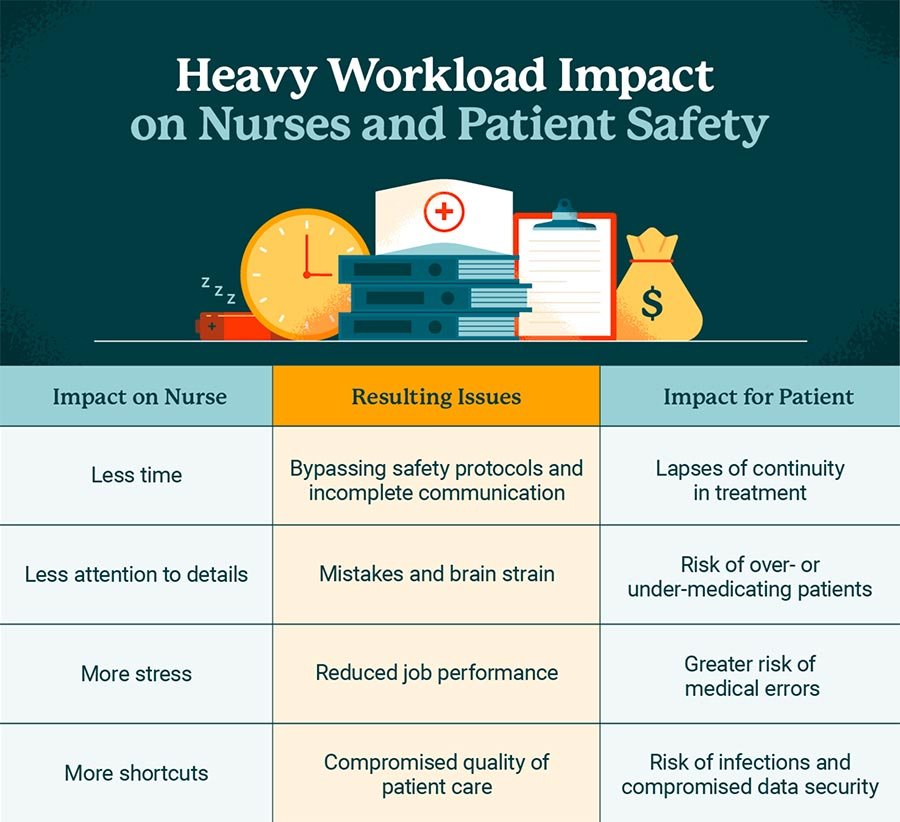
According to the NCBI¹⁰, the nursing shortage results in:
Lack of Time for Patient Tasks
Deteriorated Motivation
Stress and Burnout
Errors in Care and Medication
Policy Violations and Work-Arounds
“Shortages of hospital and clinic nursing staff also lead to a crisis in patient safety. When staff are overworked and have less time to perform routine patient tasks, errors occur.”
An ICN survey found that upwards of 90% of nurses’ associations are concerned with heavy workloads, burnout, and stress. In addition, infection rates and deaths also contribute to the nursing shortage. Nurses in close contact with infected COVID patients and have a high rate of becoming infected themselves. In the U.S., after twelve months of the pandemic there were 3,561 deaths among healthcare workers. 1,136 of these were nurses.¹¹
According to NurseJournal, at the pandemic’s start hospitals were cancelling elective surgeries to prioritize COVID-19 patients. Non-COVID patients, learning of the cancellations, avoided hospitals altogether. This reduced available funding for hospitals and resulted in staff lay-offs.¹² (In the author’s own experience in 2020, a much-needed gallbladder removal was nearly delayed at Queen’s Hospital in Hawai’i as COVID-19 cases began to overload and overwhelm the facility’s surgical and patient care resources.)
The following charts from the University of St. Augustine for Health Sciences demonstrate the looming impact of the nursing shortage on patient care among ten states.¹³
Shortages of hospital and clinic nursing staff also lead to a crisis in patient safety. When staff are overworked and have less time to perform routine patient tasks, errors occur.
Source: Pascale Carayon and Ayse Gurses, “Chapter 30: Nursing Workload and Patient Safety—A Human Factors Engineering Perspective,” Patient Safety and Quality: An Evidence-Based Handbook for Nurses.
The Remedies
Notably, some U.S. hospitals and clinics are aggressively pursuing staffing innovations, volunteerism and other forms of process optimization to meet the crisis head-on. Triaging patients and reviewing and, in some cases, rearranging patient care functions and duties are now among paramount considerations for hospital administrators. Seeking government approval for license exemptions in order to bring in needed practitioners from out-of-state has become common. Hospitals are offering bonuses to retain staff.¹⁴
The American Association of Medical Colleges points to several different approaches and potential remedies taken by healthcare facilities throughout the U.S.. These include:
The University of Arkansas for Medical Sciences (UAMS) is offering new nurses sign-up bonuses of up to $25,000.
The University of Alabama is leading teams of faculty and students to assist fragile COVID patients to improve breathing by moving patients onto their backs. The AAMC states “It typically takes nine people 45 minutes to safely turn one ICU patient.”¹⁵
The University of Massachusetts Memorial Health is pulling clinical licensees in to provide patient services, University of Maryland recruiting pharmacy students to help deliver patient bed linens, deliver specimens to labs, and deliver meal trays.
Parkland Medical in New Hampshire is offering nurses temporary contracts with higher pay rates comparable to traveling nurse salaries.
The Texas Department of State Health Services is recruiting 5,500 “medical surge staff” to address the crisis.¹⁶
The Kure Solution
Kure is a software-as-a-service digital platform that enables the user, whether it be a manager, administrator or line staff, to evaluate a problem, identify obstacles, waste and inefficiencies, and develop workable, effective solutions through its Process Optimization Path™ (Patent Pending).
The Process Optimization Path™ is a process improvement model that automates and scales process improvement throughout any organization. It’s the AI (Artificial Intelligence) that powers Kure, the only process improvement platform that integrates project management, collaboration and ROI reporting.
The Process Optimization Path™ was developed by Kure’s diverse team of process improvement, technology and education experts who have 40+ years of success using dozens of proven process improvement methodologies. Kure’s Process Optimization Path (POP) empowers everyone with the power of process improvement – no need to spend weeks in training or on expensive management consultants. It’s like TurboTax® or Waze for process improvement programs – just answer simple questions and the app does the rest.
How can the Process Optimization Path™ help solve the Nursing Shortage Crisis?
The Process Optimization Path™ combines dozens of different improvement methodologies and simplifies their application to help hospitals respond to the nursing shortage.
How can Kure help you address the nursing shortage? Following are examples of how a hospital could use the POP pathways of Quick Win, Root Cause Exploration™ and Kreative Solution™. We will summarize each path step by step leading to an improvement in nursing turnover.
Quick Win Project
A Quick Win project focuses on improvements that can be implemented rapidly at little cost or disruption. With Kure, you can quickly empower your teams to use Quality Tools like Process Maps, 5 Whys and 8 Wastes to improve patient and nurse satisfaction in a simple, powerful platform.
Following is an example of how Kure automates Quick Win Quality Improvement projects using 4 steps.
Step 1: What’s My Opportunity?
The hospital’s ongoing patient and staff satisfaction surveys show that both patients and nurses have expressed dissatisfaction with the effectiveness of the communications pertaining to patient care. Knowing that nurse-physician and patient-physician communications have been shown to affect patient outcomes, the team decided to conduct a Quick Win project to identify fast and easy improvements.
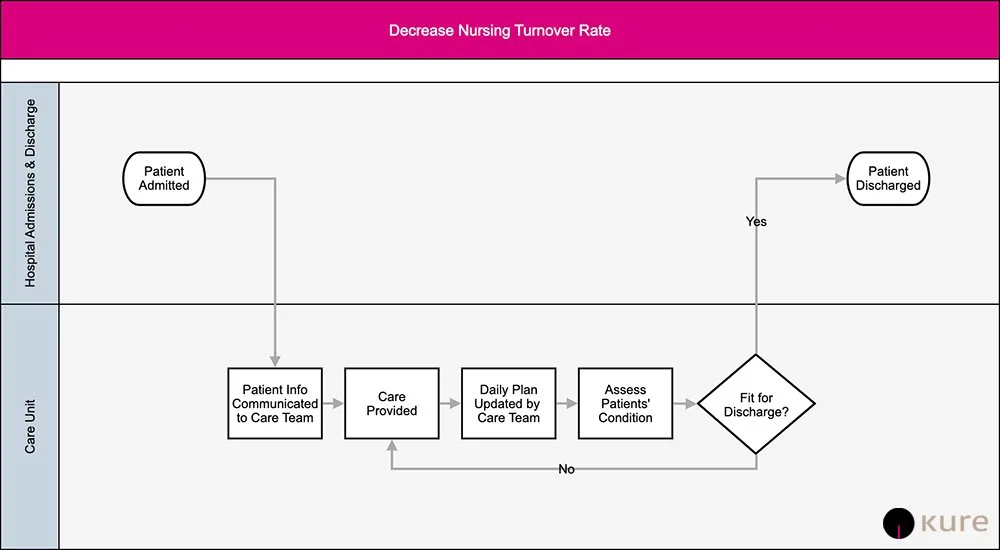
Step 2: What My Process?
The team identified the high-level process of managing patient care on a step-down unit.
A Process Walk, 8 Wastes and interviews with staff revealed the following opportunities:
Confusion on who was involved in the care team
Clear understanding of who to contact regarding patient care questions
Timely notice when the care plan or care team changed
Step 3: What’s Causing My Problem?
The team explored these opportunities and determined that the following information was not clearly defined and communicated:
Care team members,
Member role,
Updates to the care team and care plan
Step 4: What’s My Solution?
A visual handout was created of this information for care staff and a larger visual was displayed prominently in the patient’s room. This visual was updated daily.
Results:
Patient’s satisfaction for the unit rose from 67% to a 91%
Nursing satisfaction rose from 72% to 94%
Root Cause Exploration™ Project
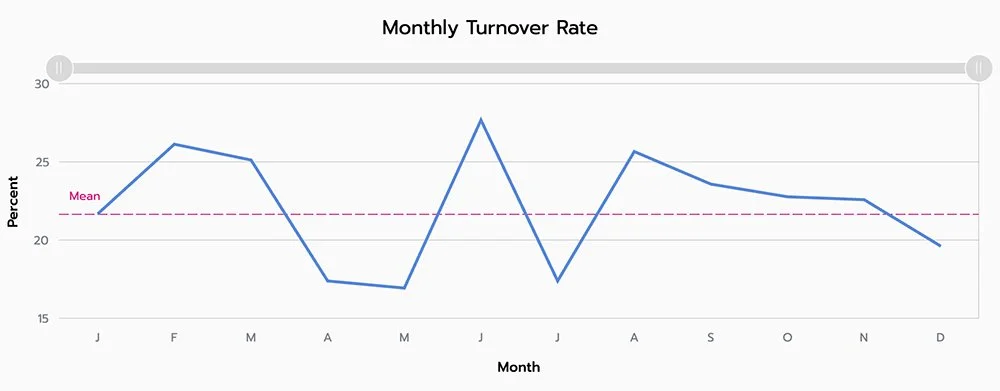
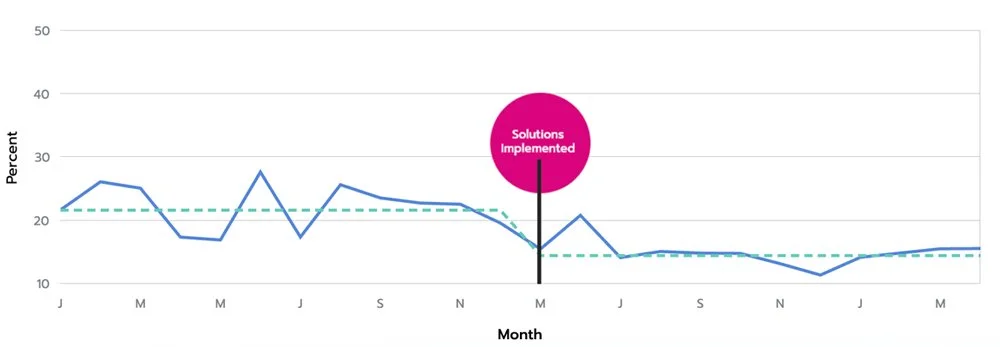
In a Root Cause Exploration™ (RCE) project, the goal is to solve a problem in which the root causes are unknown. Kure helps you explore deeper into the process to understand the root causes and reduce nursing turnover using integrated process analysis tools such as Fishbone Diagrams, Run Charts, Anomaly Detection, and Verification of Improvement.
Following is an example of how Kure automates Root Cause Analysis Quality Improvement projects using 4 steps.
Step 1: What’s My Opportunity?
Over the past year staffing shortages have increased significantly, particularly in nursing. A project was launched to reduce nurse turnover, which would impact the shortage and eventually improve hiring.
Step 2: What’s My Process?
Digging deeper revealed that:
Nurse turnover rate at 21% for the last 12 month
22% of those that leave do so in the first year
Emergency services and step down units have the highest turnover
Recent exit interviews revealed the top reasons for leaving where:
High stress
Mandatory overtime
Personal matters
Step 3: What’s Causing My Problem?
The clues gained from the previous step were explored. The goal is to identify specific, actionable causes that can be addressed with improvements.
Step 4: What’s My Solution?
Comprehensive solutions where implemented to:
Actively manage overtime and eliminate mandatory overtime
Provide flexible work schedules to encourage work/life balance
Improve care team communications
Reduce stress by providing work-life balance programs and education
Provide clarity through performance management and feedback
Redesign candidate evaluations in the hiring process
Improve communication between administration
Results: The turnover nurse turnover rate for the 2 months after the implementation dropped from 22% to 14.5%.
Kreative Solution™ Project
This path is for creating new, innovative ways to accomplish an objective. Kreative Solution™ helps teams solve problems that do not require Root Cause Exploration™, either because the causes are known or because there is no existing problem to analyze. Kure provides an easy, engaging platform for large groups to collaborate remotely and asynchronously to generate innovative ideas to increase nursing satisfaction, select the best ideas to implement and verify results.
Following is an example of how Kure automates Kreative Solution™ Quality Improvement projects using 2 steps.
Step 1: What’s My Opportunity?
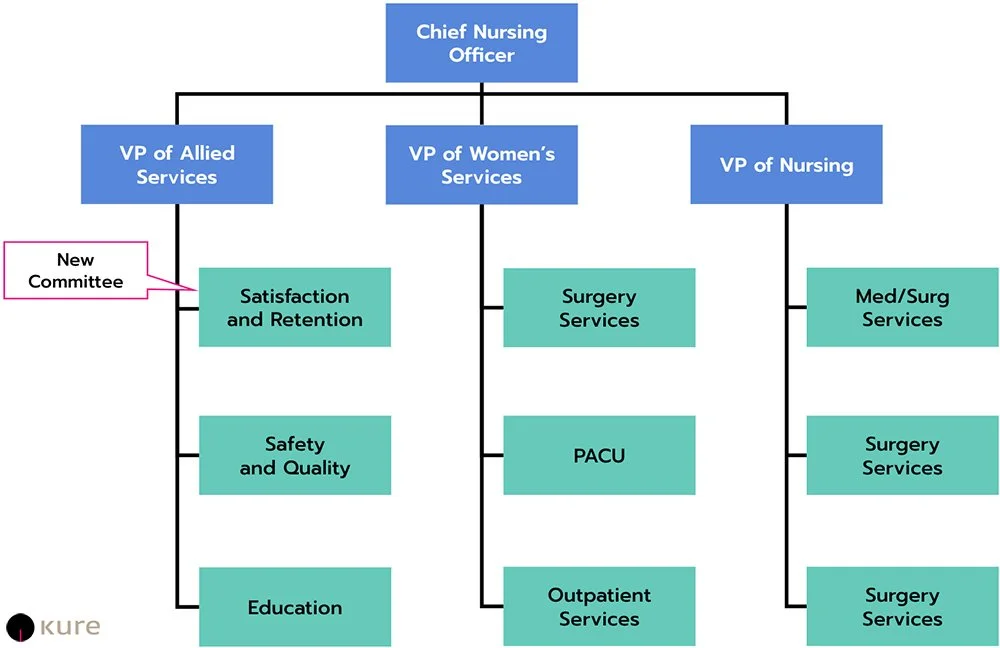
The hospital’s average nurse turnover rate for the past 18 months was 19%. They chose to focus on nursing autonomy and engagement to increase satisfaction and reduce turnover.
Step 2: What’s My Solution?
Kure guided the team to quickly generate numerous ideas and select the best. Additional committee in their shared governance model focused on nursing satisfaction and retention. Below is a summary of the model.
Results: The turnover rate declined over the next 3 months to a low of 15.7% with indications that the decline may continue.
What This Means
“Hospital care managers and staff can more easily identify staffing shortage issues, obstacles to efficient and effective patient care, workflow impediments as well as financial resource issues in order to develop workable solutions.”
With Kure and its Process Optimization Path™ (Patent Pending), hospital care managers and staff can more easily identify staffing shortage issues, obstacles to efficient and effective patient care, workflow impediments as well as financial resource issues in order to develop workable solutions.
With the system described above, a process map is created that can be shared among team members and departments, impediments are identified, root causes are determined and solutions are created either as Quick Wins or after utilization of Kure’s Root Cause Explorer where solutions require deeper analysis. The solutions can then be shared and adopted with management and staff buy-in and ongoing monitoring capabilities to ensure future compliance and success.
Conclusion
The International Council of Nurses (ICN) is promoting initiatives to help counter the nursing shortage and its effects, including ways to increase the nursing workforce.¹⁷ ICN suggests:
Protect the safety and well-being of nursing staff.
Provide psychosocial support for nurses involved in bedside care.
Commit to long-term strategies (funding, resources) to increase nursing staff.
Recruit, retain, reeducate and train nursing staff.
Improve wages and working conditions, particularly in underserved communities.
Any and all of these approaches and more may be needed at medical facilities before the pandemic fully abates. Optimization, innovation, and outside-the-box thinking are all needed.
With Kure’s SaaS (software-as-a-service) platform, medical facilities can eliminate the need to hire expensive outside management consultants and expend substantial employee time on extensive training to enable staff to identify workflow and treatment problems and generate workable solutions. Kure makes optimization accessible to all.
Supercharge your Lean Six Sigma projects and create Ethical Efficiency™ with Kure.
¹ See Association of American Medical Colleges (AAMC), Workforce/Healthcare, Patrick Boyle, Sept. 7, 2021.
² Id. See also CNN, Scottie Andrews, February 25, 2021; Nurse Journal, Gayle Morris, Oct. 12, 2021.
³ See footnote 1, supra.
⁴ See Barron’s, Matt Smith, December 27-28, 2021.
⁵ See NurseJournal, Gayle Morris, BSN, MSN, October 12, 2021.
⁶ Id.
⁷ See Vox, Dylan Scott, November 8, 2021.
⁸ Id.
⁹ Id.
¹⁰ See National Center for Biotechnology Information.
¹¹ See NurseJournal, Gayle Morris, BSN, MSN, October 12, 2021.
¹² Id.
¹³ See University of St. Augustine for Health Sciences (USAHS) “The 2021 American Nursing Shortage: A Data Study.”, May 2021. See also NurseJournal, Gayle Morris, BSN, MSN, October 12, 2021.
¹⁴ See footnote 1, supra.
¹⁵ Id.
¹⁶ See footnote 1, supra.
¹⁷ See NurseJournal, Gayle Morris, BSN, MSN, October 12, 2021.