Healthcare System Decreased Initial Payment Denials By 26% With Kure
PROJECT SUMMARY
Problem: A healthcare system found itself facing a substantial challenge: a staggering $3.4 million in monthly losses due to initial payment denials. These denials disrupted cash flow, increased staff workload, and jeopardized the efficiency of their operation.
The system turned to Kure, the AI-powered process improvement software. Kure guided the team step by step to reduce initial payment denials from an average of $3.4 million to $2.5 million per month, a 26% improvement that saved $900K per month.
The Problem
In the fast-paced world of healthcare, keeping finances in check is just as important as delivering high-quality patient care. But one healthcare system found itself in a tough spot—losing a massive $3.4 million every month due to initial payment denials from insurance providers.
These denials weren’t just hitting their bottom line. They were clogging up workflows, overloading staff, and making it harder to provide efficient care. Without a clear, organized approach to handling insurance authorizations and referrals, they risked falling even further behind.
The organization knew they had to act fast. They assembled a team of skilled professionals led by a project leader using Kure, an AI-powered process improvement software. Kure guided the team step by step using the DMAIC (Define, Measure, Analyze, Improve, Control) framework, providing AI-driven insights, real-world examples, and expert recommendations to accelerate the project and keep them focused on the best solutions.
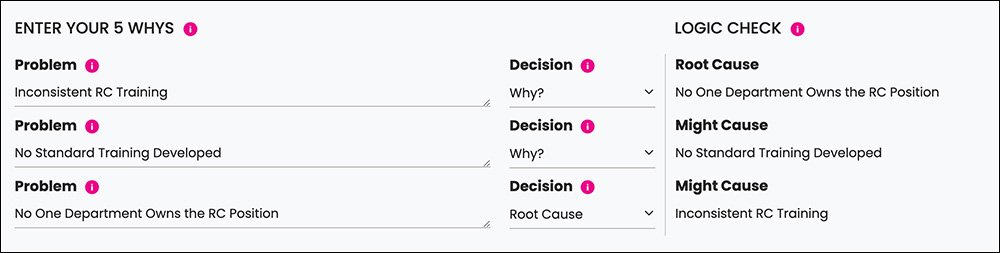
The Root Causes
With Kure leading the way, the team dug into the data and pinpointed the real issues behind the overwhelming number of payment denials. Here’s what they found:
No Clear Ownership – No single department was in charge of overseeing referrals, leading to confusion and lack of accountability.
Scattered Reporting – Referral coordinators were spread out across different teams, making workflows inconsistent.
No Standard Process – Every department handled referrals and authorizations differently, creating inefficiencies and unnecessary delays.
It became clear that without a unified, structured approach, the organization would continue to struggle.
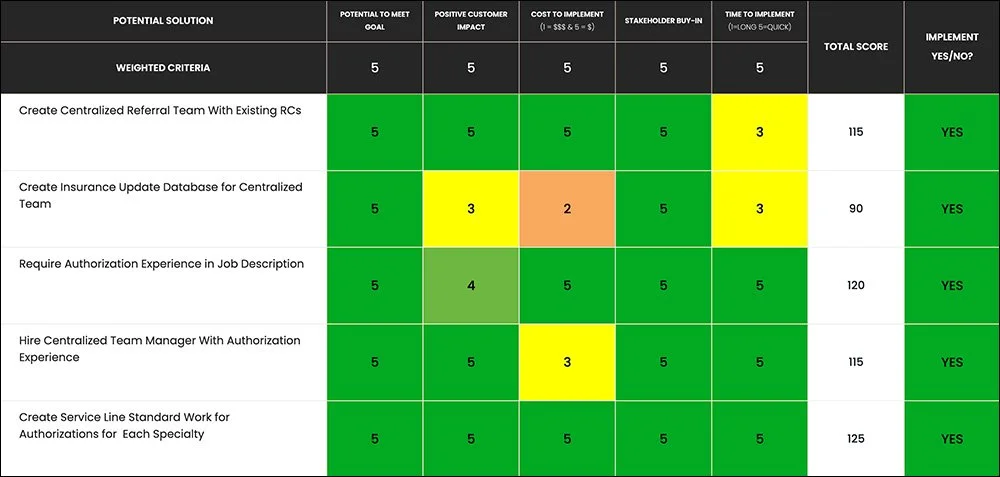
The Solutions
With Kure’s AI-driven guidance, the team crafted a plan to fix these issues at the source. Kure provided customized recommendations and real-world examples that helped them move quickly and make the right decisions.
Here’s what they implemented:
Centralized Referral Team – All referral coordinators were brought together under one team, ensuring consistent processes and clear communication.
Insurance Update Database – A single source of truth was created to track insurance policy changes and avoid preventable denials.
New Hiring Standards – Authorization experience became a requirement for new hires, making sure staff had the right expertise from day one.
Dedicated Leadership – A manager with deep experience in authorizations was brought in to lead the team and provide ongoing guidance.
Standardized Processes – The team developed step-by-step procedures for handling referrals and authorizations, reducing errors and streamlining approvals.
With Kure’s AI-driven workflow, the team stayed on track, received real-time data insights, and made fact-based decisions faster than ever.
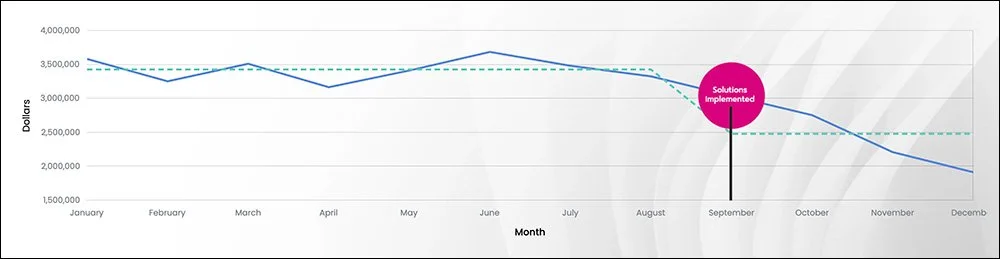
The Results
The impact was immediate and game-changing! The organization cut payment denials by 26%, reducing monthly losses from $3.4 million to $2.5 million, saving an incredible $900K per month.
But the benefits went beyond just the numbers:
More Efficient Workflows – With standardized processes in place, teams worked smarter, not harder.
Happier, More Confident Staff – Referral coordinators finally had clear expectations and strong leadership, making their workdays smoother.
Improved Collaboration – The centralized system brought teams together, boosting teamwork and knowledge sharing across departments.
By following Kure’s AI-guided process, the team wrapped up their project 3x faster than traditional methods—turning a frustrating challenge into a huge success.
Conclusion
This success story highlights how Kure’s AI-powered process improvement software empowers teams to fix complex challenges faster and more effectively. By pinpointing the root causes, providing expert recommendations, and guiding the team through the best solutions, Kure helped this healthcare system regain financial stability and streamline operations.
Now, with efficient workflows and a skilled, well-supported team, this organization is better positioned for long-term success—ensuring patients get the care they need without financial roadblocks.
With Kure, solving big problems doesn’t have to be overwhelming. Faster projects, smarter decisions, and better results—it’s all possible with AI-driven process improvement!
*We value our clients’ confidentiality. While we’ve changed their names, the results are real.