Hoyleton Youth & Family Services Reduces Invalid Claims By 100% With With Kure
PROJECT SUMMARY
Business Case
Increase time efficiency, reduce duplication of work, reduce rework due to defects, increase worker satisfaction
Root Cause Analysis
CIS has more built-in mistake proofing, preventing errors
Solutions Implemented
Migrate all BH salesforce work to CIS
Project Results
Greatly reduced invalid claims from 41% to 0%
Introduction
Hoyleton Youth & Family Services is a nonprofit providing essential mental and behavioral health services, including counseling, crisis intervention, foster care, therapeutic residential care, and Hispanic community support. These services, funded through grants or insurance, including Medicaid, face challenges such as limited funding, staffing shortages, and complex billing and documentation requirements. Reimbursement delays due to these complexities can strain financial resources and impact the ability to provide critical services.
The Challenge
Insurance-billed services come with unique documentation and billing requirements that vary by insurer. Hoyleton's claiming systems struggled to process a significant portion of claims within the billing cycle, leading to a 25% claim invalidation rate. This created substantial rework for staff, from service verification specialists to revenue cycle analysts.
The Approach
A team of skilled professionals, led by an experienced project manager undergoing Lean Six Sigma Green Belt Training & Certification from GLSS, was assembled to tackle the issue. The team also utilized Kure, an AI-powered process improvement software, to streamline project work and focus more on problem-solving.
The Root Causes
Behavioral health claims were processed using two systems: Salesforce and CIS. Using the 5 Whys technique they determined a potential root cause was that CIS seemed to have more ability to catch error than Salesforce.
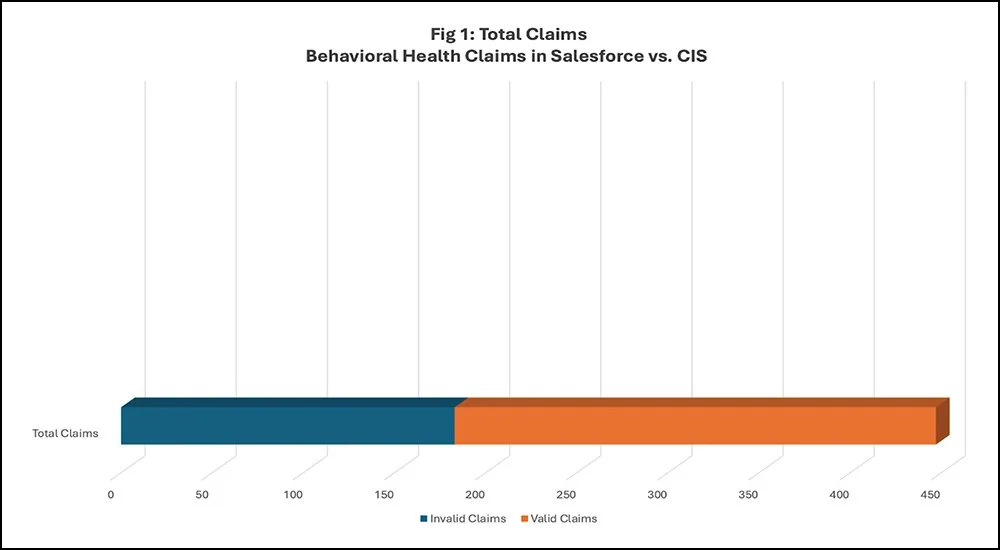
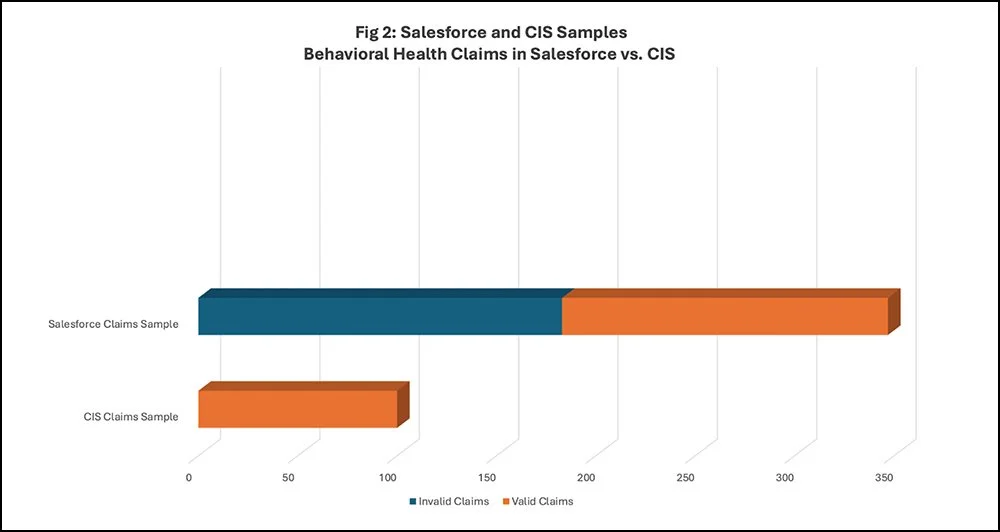
To confirm this, analysis of nearly 500 claims showed that about 41% were invalid and could not be submitted for reimbursement (Figure 1). Salesforce accounted for 53% of these invalid claims, while CIS identified none (Figure 2). The root cause analysis revealed that CIS had superior error-proofing and integration with the Medicare site, MEDI, ensuring accurate billing.
The Solution
The project team decided that migrating all behavioral health claims to CIS was more efficient than reconfiguring Salesforce. CIS had a robust system for handling insurance claims and verifying client eligibility through MEDI, leading to fewer errors.
The Results
In a pilot migration, CIS processed claims with zero invalid claims. The claims were successfully processed and paid by the reimburser, confirming a 100% improvement in invalid claims. Full migration is scheduled for July 2024.
Conclusion
When addressing revenue cycle management issues, it's crucial to identify all sources of errors and avoid temporary fixes that don't address the root cause. Comprehensive information collection helps differentiate between symptoms and root causes of inefficiencies. Kure was key to this project's success, equipping the Hoyleton team with the necessary guidance, knowledge, and tools to effectively diagnose and resolve billing issues. This ensured a smooth transition from problems to solutions, resulting in a remarkable 100% reduction in invalid claims. With Kure, Hoyleton not only solved their immediate problem but also established a foundation for future efficiency and success.
This Lean Six Sigma Case Study was completed in collaboration with Illuminative Strategies, Inc., a management consulting firm offering business process optimization, project management, and more to clients throughout the United States & Canada.